National Pain Week 2024
National Pain Week is Australia’s annual awareness event for chronic pain. National Pain Week takes place in the last week of July each year and aims to support and provide awareness to the 3.6 million Australian’s living with chronic pain.
This week The Hopkins Centre together with Griffith Inclusive Futures: Reimagining Disability, has teamed up with Dr Nicholas Aitcheson (Rehabilitation and Pain Specialist, at Metro South Pain Rehabilitation Centre) and Kimberly Talaber (Physiotherapist and PhD candidate with a special interest in pain) to explain acute and chronic pain, how the body feels pain, current treatment options and lifestyle solutions.
Join us for our special Hopkins Hour virtual Event on 24 July, 12-1.30pm.
Acute pain vs chronic pain
Picture a child with a band-aid vs a person with pills and injections and ongoing pain.
Our upbringing often tells us that pain is associated with body damage and that we need to rest and get other people’s help to fix it. This works for acute pain, but in chronic pain we need to take control of our own lives, actively work on changing our bodies and minds and find new ways of existing, instead of trying to return to a life that we miss and are nostalgic about.
Relying on rest leads to deconditioning, isolation and weakness. Relying on other people can lead to dynamics of disempowerment. Similarly, relying on medications and surgery leads to reliance on interventions that promise only temporary relief and can have serious side effects.
Check with your health professional that you are safe to proceed (most people with chronic pain are sore but stable and are safe to move). Then gently and progressively start to actively create a new life for yourself.
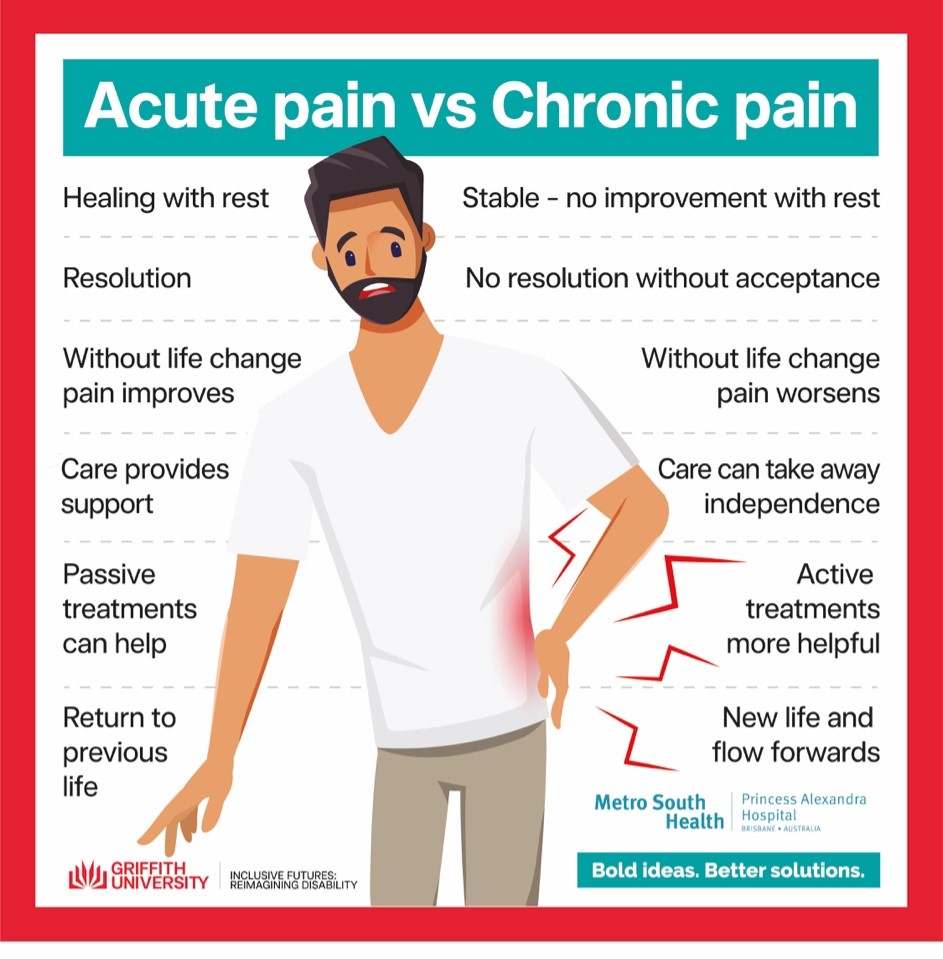
| Acute | Chronic |
| Healing with rest Resolution Without life change pain improves Care provides support Passive treatments can help Return to previous life |
Stable – no improvement with rest No resolution without acceptance Without life change pain worsens Care can take away independence Active treatments more helpful New life and flow forwards |
Chronic pain is like a malfunctioning, overly sensitive alarm system.
In acute pain our alarm system is working well. If there is body damage or the potential for damage then we feel it and do something about it.
In chronic pain the alarm system reacts too strongly with only very small input. It is like a smoke alarm going off when you are cooking toast or a car alarm going off when it rains. The alarm does not accurately represent the threat to the body. Often in chronic pain the body is stable and safe but the alarm system is still going.
The brain drives the pain
Pain is felt in the brain. What we are starting to understand is that our mood and the way we think about pain affects the strength of the pain signal that reaches our brain. If we are really worried about the meaning of the pain then the pain tends to be worse.
If you can successfully change your thinking around pain then you can “decrease the volume” on the pain signal by affecting the pain signal transmission in the spinal cord and brain.
Here are some thoughts that may be unhelpful and some ways to address them:
My body is broken. It wouldn’t be so painful unless there was something seriously wrong.
Pain can exist without damage. Amount of pain does not reflect amount of damage. Think “sore but safe”, “hurt not harm”
This pain means I’m never going to be able to do anything I enjoy again.
Think of the things you can enjoy now even with your current condition. Enjoy those things and gently find ways to expand the things you enjoy.
My back is so sore that I’ll probably be in a wheelchair soon.
Pain is often not indicative of damage, especially not the kind of nerve damage that leads to paralysis.
I might not be able to work for much longer because of this pain and then I won’t be able to support myself or my family.
These are reasonable thoughts to have, however worrying about them can make pain worse. Trying to address unhelpful, repetitive thoughts can help with your pain.
I need to protect my body. That’s why I keep my muscles so tense.
Muscle tension in itself usually leads to worsening of chronic pain. Gentle relaxation and movement is much more beneficial.
Low mood, anxiety, excessive worry, poor sleep all increase pain as well, so dealing with these tends to improve pain.
All causes of pain are valid
PhD Candidate Kim Talaber's survey collected nearly 100 responses from people with SCI-related pain describing what they think the cause of their pain was. There was a spectrum of descriptions, indicating that people have different understandings of what causes pain. This could be due to information from various health professionals, perhaps using the internet to interpret, as well as personal belief frameworks.
Ultimately, regardless of what you think is causing your pain, your pain experience is valid and worth sharing with a trusted health professional. Someone can have different pain experiences even within the same body area. The nature of chronic pain (pain persisting >3 months) is that it can change and morph, expanding into body areas that weren’t the original problem. This is particularly troublesome in those with neuropathic pain following SCI; despite a lack of sensation and movement, someone can experience harsh, severe pain below the level of injury. People with an SCI may experience several different pains throughout their body, and this tile reinforces that all pain experiences are valid and worth advocating for.

Advocating for yourself can look like...
Kim's survey collected responses about which management strategies people with SCI-related pain currently use or have previously used, and how effective they feel these strategies are/were for managing their pain.
Strategies included:
- Medication (over-the-counter & prescription),
- Cannabis therapy,
- Surgery/procedure,
- Physical activity/exercise program,
- Psychology,
- Physiotherapy,
- Occupational therapy,
- Social work input,
- Using particular piece of equipment,
- Spiritual/religious practices.

The message with this tile is the importance for people to feel empowered to try different strategies, even if an experience in the past was not successful. Due to the malleable nature of chronic pain, a strategy used previously might be more or less appropriate now. This tile represents speaking to your trusted healthcare professional if you are interested in trying a new strategy, knowing that lots of people with SCI-related pain have had success in managing their pain with a variety of strategies.
Find out more by reading the Pain Revolution fact sheets